ده الجزء الثانى من
angina
للرجوع للجزء الاول اضغط هنا
http://werdoctors.blogspot.com/2012/03/angina.html
What are other causes of chest pain?
In caring for patients with chest pain, the doctor distinguishes whether the pain is related to a lack of oxygen to the heart muscle (as in angina or heart attack), or is due to another process. Many conditions are considered that can cause chest pain which is similar to that of a heart attack or angina. Examples include the following:
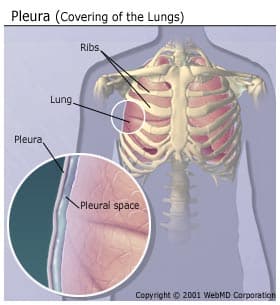
- Pleuritis (pleurisy): Inflammation of the lining of the lungs (pleuritis) causes sharp chest pain, which is aggravated by deep breathing and coughing. Patients often notice shortness of breath, in part due to their shallow breathing to minimize chest pain. Viral infections are the most common causes of pleurisy. Other systemic inflammatory conditions, such as systemic lupus, can also cause pleurisy.

- Pericarditis: Pericarditis is inflammation of the lining around the heart. Symptoms of pericarditis are similar to that of pleuritis.


-

- Pneumonia: Pneumonia (bacterial infection of the lung) causes fever and chest pain. Chest pain in bacterial pneumonia is due to an irritation or infection of the lining of the lung (pleura).

- Pulmonary embolism: blood clots travel from the veins of the pelvis or the lower extremities to the lung, the condition is called pulmonary embolism. Pulmonary embolism can cause death of lung tissue (pulmonary infarction). Pulmonary infarction can lead to irritation of the pleura, causing chest pain similar to pleurisy. Some common causes of blood clots in these veins is deep vein thrombosis (prolonged immobility, recent surgery, trauma to the legs, or pelvic infection).


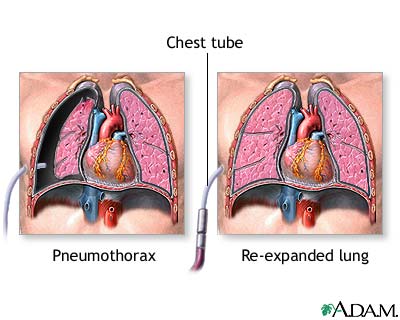
- Pneumothorax: Small sacs in the lung tissue (alveoli) can spontaneously burst, causing pneumothorax. Symptoms of pneumothorax include sudden, severe, sharp chest pain and shortness of breath. One common cause of pneumothorax is severe emphysema.
-

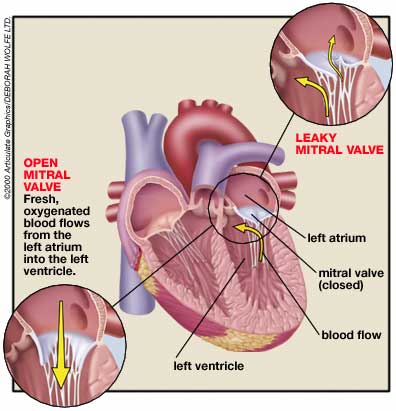
- Mitral valve prolapse: Mitral valve prolapse is a common heart valve abnormality, affecting 5% to 10% of the population. MVP is especially common among women between 20 to 40 years of age. Chest pain with MVP is usually sharp but not severe. Unlike angina, chest pain with MVP rarely occurs during or after exercise, and usually will not respond to nitroglycerin.
-

- Aortic dissection: The aorta is the major vessel delivering blood from the left ventricle to the rest of the body. Aortic dissection (tearing of the aorta wall) is a life-threatening emergency. Aortic dissection causes severe, unrelenting chest and back pain. Young adults with aortic dissection usually have Marfan's syndrome, an inherited disease in which an abnormal form of the structural protein called collagen causes weakness of the aortic wall. Older patients develop aortic dissection typically as a result of chronic, high blood pressure, in addition to generalized hardening of the arteries (arteriosclerosis).

- Costochondritis, rib fractures, muscle strain or spasm: Pain originating from the chest wall may be due to muscle strain or spasm, costochondritis, or rib fractures. Chest wall pain is usually sharp and constant. It is usually worsened by movement, coughing, deep breathing, and direct pressure on the area. Muscle spasm and strain can result from vigorous, unusual twisting and bending. The joints between the ribs and cartilage next to the breastbone can become inflamed, a condition called costochondritis. Fractured ribs resulting from trauma or cancer involvement can cause significant chest pain.

- Nerve compression: Compression of the nerve roots by bone spurs as they exit the spinal cord can cause pain. Nerve compression can also cause weakness and numbness in the upper arm and chest.

- Shingles (herpes zoster infection of the nerves): Shingles is nerve irritation from the infection, which can cause chest pain days before any typical rash appears.

- Esophageal spasm and reflux: The esophagus is the long muscular tube connecting the mouth to the stomach. Reflux, or regurgitation of stomach contents and acid into the esophagus can cause heartburn and chest pain. Spasm of the muscle of the esophagus can also cause chest pain which can be indistinguishable from chest pain caused by angina or a heart attack. The cause of esophageal muscle spasm is not known. Pain of esophageal spasm can respond to nitroglycerin in a similar manner as angina.


- Gallbladder attack (gallstones): Gallstones can block the gallbladder or bile ducts and cause severe pain of the upper abdomen, back and chest. Gallbladder attacks can mimic the pain of angina and heart attack.

- Anxiety and panic attacks: Anxiety, depression, and panic attacks are frequently associated with chest pain lasting from minutes to days. The pain can be sharp or dull. It is usually accompanied by shortness of breath, or the inability to take a deep breath. Emotional stress can aggravate chest pain, but the pain is generally not related to exertion, and is not relieved by nitroglycerin. These patients often breath too fast (hyperventilate), causing lightheadedness, numbness, and tingling in the lips and fingers. Coronary artery disease risk factors are typically absent in these patients. Since there is no test for panic attacks, patients with chest pain usually undergo tests to exclude coronary artery disease and other causes of chest pain.
What are the treatment options for angina patients?
Treatment options include:
- rest,
- medications (nitroglycerin, beta blockers, calcium channel blockers),
- percutaneous transluminal coronary angioplasty (PTCA), or
- coronary artery bypass graft surgery (CABG).
Angina medications
Nitroglycerin
Resting, nitroglycerin tablets (placed under the tongue), and nitroglycerin sprays all relieve angina by reducing the heart muscle's demand for oxygen. Nitroglycerin also relieves spasm of the coronary arteries and can redistribute coronary artery blood flow to areas that need it most. Short-acting nitroglycerin can be repeated at five minute intervals. When 3 doses of nitroglycerin fail to relieve the angina, further medical attention is recommended. Short-acting nitroglycerin can also be used prior to exertion to prevent angina.
Longer-acting nitroglycerin preparations, such as Isordil tablets, Nitro-Dur transdermal systems (patch form), and Nitrol ointment are useful in preventing and reducing the frequency and intensity of episodes in patients with chronic angina. The use of nitroglycerin preparations may cause headaches and lightheadedness due to an excess lowering of blood pressure.
Beta Blockers
Beta blockers relieve angina by inhibiting the effect of adrenaline on the heart. Inhibiting adrenaline decreases the heart rate, lowers the blood pressure, and reduces the pumping force of the heart muscle, all of which reduce the heart muscle's demand for oxygen. Examples of beta blockers include:
- acebutolol (Sectral)
- atenolol (Tenormin)
- bisoprolol (Zebeta)
- metoprolol (Lopressor, Lopressor LA, Toprol XL)
- nadolol (Corgard)
- propranolol (Inderal)
- timolol (Blocadren)
Side effects include of beta blockers include:
- worsening of asthma,
- excess lowering of the heart rate and blood pressure,
- depression,
- fatigue,
- impotence,
- increased cholesterol levels, and
- shortness of breath due to diminished heart muscle function (congestive heart failure).
Calcium Channel Blockers
Calcium channel blockers relieve angina by lowering blood pressure, and reducing the pumping force of the heart muscle, thereby reducing muscle oxygen demand. Calcium channel blockers also relieve coronary artery spasm. Examples of calcium channel blockers include:
- amlodipine (Norvasc)
- bepridil (Vascor)
- diltiazem (Cardizem)
- felodipine (Plendil)
- isradipine (Dynacirc)
- nicardipine, (Cardene)
- nifedipine (Adalat, Procardia)
- nimodipine (Nimotop)
- nisoldipine (Sular)
- verapamil (Calan)
Side effects of calcium channel blockers include:
- swelling of the legs,
- excess lowering of the heart rate and blood pressure, and
- depressing heart muscle function.
Other anti-anginal drugs
Ranolazine (Ranexa) is indicated for the treatment of chronic angina. Ranexa may be used with beta-blockers, nitrates, calcium channel blockers, antiplatelet therapy, lipid-lowering therapy, ACE inhibitors, and angiotensin receptor blockers.
Why is it important to establish the diagnosis of angina?
Angina is usually a warning sign of the presence of significant coronary artery disease. Patients with angina are at risk of developing a heart attack (myocardial infarction). A heart attack is the death of heart muscle precipitated by the complete blockage of a diseased coronary artery by a blood clot.
During angina, the lack of oxygen (ischemia) to the heart muscle is temporary and reversible. The lack of oxygen to the heart muscle resolves and the chest pain disappears when the patient rests. In contrast, the muscle damage in a heart attack is permanent. The dead muscle turns into scar tissue when healed. A scarred heart cannot pump blood as efficiently as a normal heart, and can lead to heart failure.
Up to 25% of patients with significant coronary artery disease have no symptoms at all, even though they clearly lack adequate blood and oxygen supply to the heart muscle. These patients have "silent" angina. They have the same risk of heart attack as those with symptoms of angina.
How is angina diagnosed?
The electrocardiogram (EKG, ECG) is a recording of the electrical activity of the heart muscle, and can detect heart muscle which is in need of oxygen. The EKG is useful in showing changes caused by inadequate oxygenation of the heart muscle or a heart attack.
Exercise stress test
In patients with a normal resting EKG, exercise treadmill or bicycle testing can be useful screening tools for coronary artery disease. During an exercise stress test (also referred to as stress test, exercise electrocardiogram, graded exercise treadmill test, or stress ECG), EKG recordings of the heart are performed continuously as the patient walks on a treadmill or pedals on a stationary bike at increasing levels of difficulty. The occurrence of chest pain during exercise can be correlated with changes on the EKG, which demonstrates the lack of oxygen to the heart muscle. When the patient rests, the angina and the changes on the EKG which indicate lack of oxygen to the heart can both disappear. The accuracy of exercise stress tests in the diagnosis of significant coronary artery disease is 60% to 70%. If the exercise stress test does not show signs of coronary artery disease, a nuclear agent (thallium) can be given intravenously during exercise stress test. The addition of thallium allows nuclear imaging of blood flow to different regions of the heart, using an external camera. A reduced blood flow in an area of the heart during exercise, with normal blood flow to the area at rest, signifies significant artery narrowing in that region of the heart.
Stress echocardiography
Stress echocardiography combines echocardiography (ultrasound imaging of the heart muscle) with exercise stress testing. Like the exercise thallium test, stress echocardiography is more accurate than an exercise stress test in detecting coronary artery disease. When a coronary artery is significantly narrowed, the heart muscle supplied by this artery does not contract as well as the rest of the heart muscle during exercise. Abnormalities in muscle contraction can be detected by echocardiography. Stress echocardiography and thallium stress tests are both about 80% to 85% accurate in detecting significant coronary artery disease.
When a patient cannot undergo exercise stress test because of neurological or orthopedic difficulties, medications can be injected intravenously to simulate the stress on the heart normally brought on by exercise. Heart imaging can be performed with a nuclear camera or echocardiography.
Cardiac catheterization
Cardiac catheterization with angiography (coronary arteriography) is a technique that allows x-ray pictures to be taken of the coronary arteries. It is the most accurate test to detect coronary artery narrowing. Small hollow plastic tubes (catheters) are advanced under x-ray guidance to the openings of the coronary arteries. Iodine contrast "dye" is injected into the arteries while an x-ray video is recorded. Coronary arteriography gives the doctor a picture of the location and severity of coronary artery disease. This information can be important in helping doctors select treatment options.
CT coronary angiogram
CT coronary angiography is procedure that uses an intravenous dye that contains iodine, and CT scanning to image the coronary arteries. While the use of catheters is not necessary (thus the term "noninvasive" test applies to this procedure), there are still some risks involved, including the following:
- Patients allergic to iodine
- Patients with abnormal kidney function
- Radiation exposure which is similar to, if not greater than, that received with a conventional coronary angiogram.
Nonetheless, this is generally a very safe test for most people. It is a major tool in the diagnosis of coronary artery disease in patients:
- at high risk for developing coronary disease (cigarette smokers, those with genetic risk, high cholesterol levels, hypertension, or diabetes),
- who have unclear results with exercise stress tests or other testing, or
- who have symptoms suspicious of coronary disease
لمتابعتنا على الفيس بوك
اضغط هنا
reference
medicinet
medlineplus








No comments:
Post a Comment